Up to two-thirds of people don’t respond fully to their first prescribed antidepressant.1 If you’re in this situation, you’re not alone — switching antidepressants is a common and important part of finding the right treatment.
Changing medications is not a sign of failure, but rather a step toward discovering what works best for you. And because antidepressants affect brain chemistry, the transition should always be made under medical supervision to avoid complications.
This guide explains why switching may be recommended, the most common methods doctors use, what timelines to expect and practical tips to make the transition safer and smoother.
Key Takeaways
Switching antidepressants is common and part of the treatment process.
Different strategies are chosen based on the medications involved (direct switch, cross-taper, taper and switch, augmentation).
Withdrawal symptoms and side effects may overlap during the transition.
New medications may take several weeks or months to show full effect.
Close medical supervision makes switching safe and more effective.
Why switch antidepressants?
People may switch antidepressants for many reasons, including:
Poor response: It may be wise to try something new if your symptoms don’t improve after a full trial.
Tolerance: The medication may become less effective over time.
Side effects: You may experience unwanted side effects such as weight changes, sleep issues, sexual dysfunction or emotional blunting (a sense of numbness to both positive and negative feelings).2,3
Drug interactions: You will need an antidepressant that does not have adverse interactions with any other medications you are on.
Life events: Pregnancy, breastfeeding, menopause or family planning may affect your choices.
Convenience: For example, you consider options with once-daily dosing and simpler regimens to make treatment easier.
New options: Advances in antidepressants may offer better-tolerated or faster-acting alternatives than what you currently take.
Common Strategies to Switch Antidepressants
There are different ways to approach changing antidepressants, including:4,5
Direct switch: When you stop taking your old antidepressant and start your new one the next day.
Cross-taper: When you gradually lower (taper) the dose of your old antidepressant and slowly start the new one at the same time.
Taper and switch (without a washout period): This means you taper and stop your old antidepressant, and then, once you’ve fully stopped your old antidepressant, you start the new one the next day.
Taper and switch (with a washout period): This means you taper and stop your old antidepressant, then wait a period of time (days or weeks) before starting the new medication. This strategy is used when the two antidepressants have the potential to interact with each other.
Augmentation: This means adding another medication to the one you’re currently taking. This is typically a strategy for treatment-resistant depression.
How long the tapering period lasts depends on the half-life of your medication. A drug’s half-life is how long it takes for the drug’s initial concentration in your body to decrease by half. This can vary person to person based on age, digestive function, prescribed dosage and other factors.
Switching Antidepressants Chart
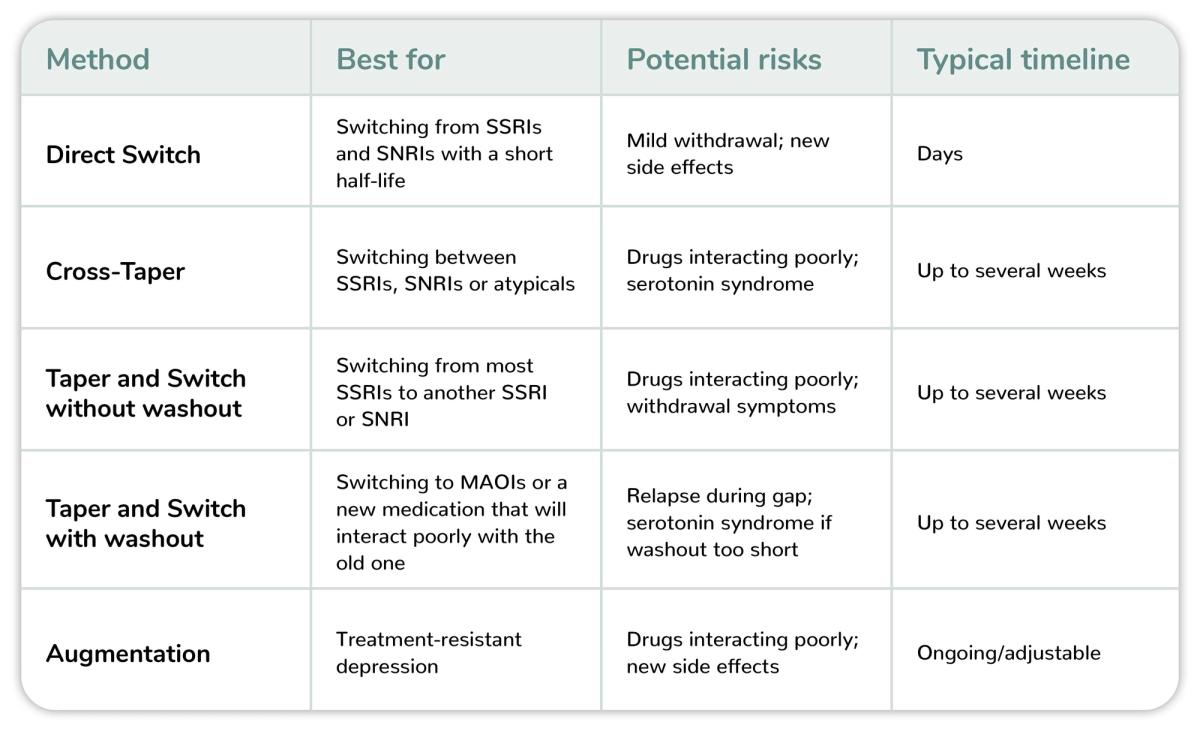
Chart Key — Antidepressants6, 7
SSRI — Selective serotonin reuptake inhibitor: fluoxetine (Prozac), sertraline (Zoloft), escitalopram (Lexapro)
SNRI — Serotonin–norepinephrine reuptake inhibitor: venlafaxine (Effexor XR), duloxetine (Cymbalta), desvenlafaxine (Pristiq)
MAOI — Monoamine oxidase inhibitor: phenelzine (Nardil), tranylcypromine (Parnate), isocarboxazid (Marplan)
TCA — Tricyclic antidepressant: amitriptyline, nortriptyline (Pamelor), imipramine (Tofranil)
Atypicals: bupropion (Wellbutrin), mirtazapine (Remeron), trazodone
How long does it take to work when switching antidepressants?
The adjustment period can vary based on your personal health and the medication class of the antidepressant. Some people notice improvement within the first two weeks, but it typically takes at least four to eight weeks — or up to several months — for a new medication to take full effect.8
Keep in mind that withdrawal symptoms from the old medication may overlap with side effects from the new one, so some people feel worse before they feel better.

Convenient, affordable anxiety and depression treatment online.
Your mental health is important. Start your secure, private online doctor consultation and get treatment for $25/month.
Get StartedWhat to expect when switching antidepressants?
While every patient is different, there are certain risks to watch for when switching antidepressants.
More common risks include:
Any side effects from your new medication.
General withdrawal symptoms such as nausea, dizziness and mood swings.
Less common risks include:
Discontinuation syndrome: This is a type of withdrawal typically associated with antidepressant medication and can cause insomnia, nausea and flu-like symptoms.9
Brain zaps: These are brief sensations of mild electric shock, typically felt in a patient’s head.10, 11
Serotonin syndrome: This occurs when different medications create high levels of serotonin in the body. Symptoms include insomnia, confusion, high blood pressure, sweating, headaches, diarrhea and more. Mild serotonin syndrome may go away on its own, while severe cases require medical treatment.12
Week-by-Week Overview
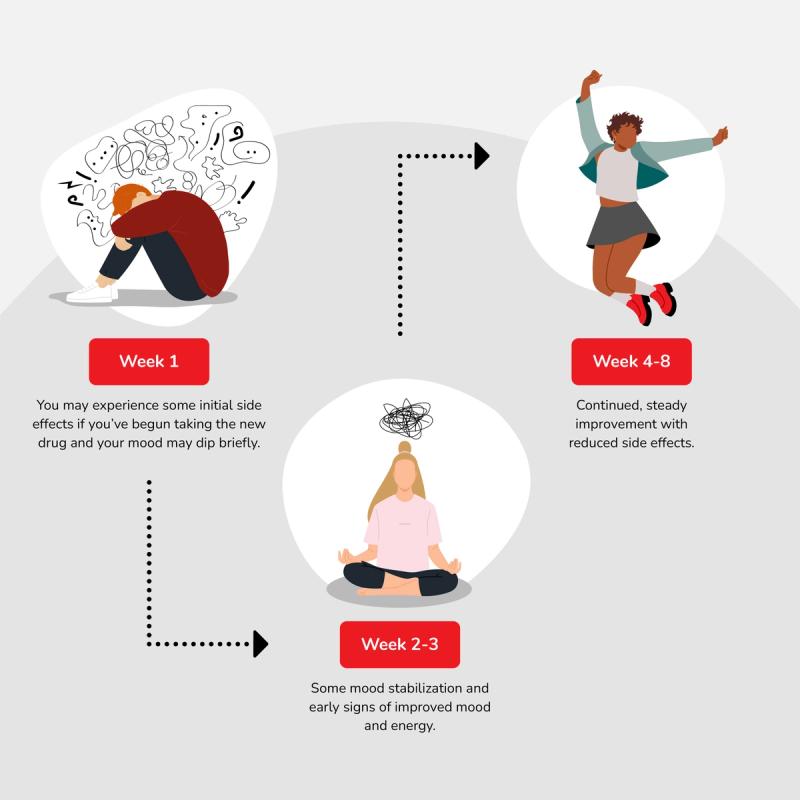
While each patient’s experience is unique, the first several weeks of antidepressant transition may look like this:13
Week 1: You may experience some initial side effects if you’ve begun taking the new drug and your mood may dip briefly.
Weeks 2–3: Some mood stabilization and early signs of improved mood and energy.
Weeks 4–8+: Continued, steady improvement with reduced side effects.
Tips & Considerations
Switching antidepressants safely is a team effort between you and your provider. Keep these best practices in mind to support your mental health:
Track symptoms daily: Monitor your mood, sleep, energy level and daily appetite in a journal or app.
Watch for red flags: Stay vigilant for signs of withdrawal, discontinuation syndrome or serotonin syndrome.
Support your body: Get consistent sleep; eat healthy, balanced meals; add light exercise to your daily routine; and limit alcohol and caffeine.
Lean on support: Ask a trusted friend or family member to check in during this transition period.
Follow the plan: Never alter your dose or skip your medication without your doctor’s guidance.
Questions to Ask Your Doctor
Before making any medication change, it’s important to have a clear plan with your provider. Asking these questions can help you understand the process, set realistic expectations and feel more confident during the transition:
Why am I switching medications?
Which method will I use? (i.e. direct switch, cross-taper, switch and taper, augmentation)
What side effects or withdrawal symptoms should I expect?
How long before I know if the new medication is working?
What’s my next step if this switch isn’t effective?
How RedBox Rx can help

RedBox Rx makes it easy and affordable to receive antidepressants and other mental health treatments. We offer secure, private online consultations with licensed providers focused on your health.
Benefits of RedBox Rx include:
Transparent, affordable, flat rates.
Medications for $25 per month (with purchase of three-month supply).
$35 consultations with a U.S. licensed medical professional.
No insurance required. No membership fees. HSA and FSA eligible.
No office wait times or scheduling issues typical with physical medical practices.
FREE shipping directly to you. Monthly and quarterly subscriptions available.
Get started on your mental health treatment journey with our online assessment for depression.
If you are experiencing suicidal or self-harm thoughts, please reach out immediately to a health care provider, call the National Suicide Prevention Lifeline at 1-800-273-8255, or call the Suicide and Crisis line at 988.